Outcomes

VAAACares® delivers measurable results and positive outcomes. We have a proven track record and our team is focused on achieving goals for you and your members.
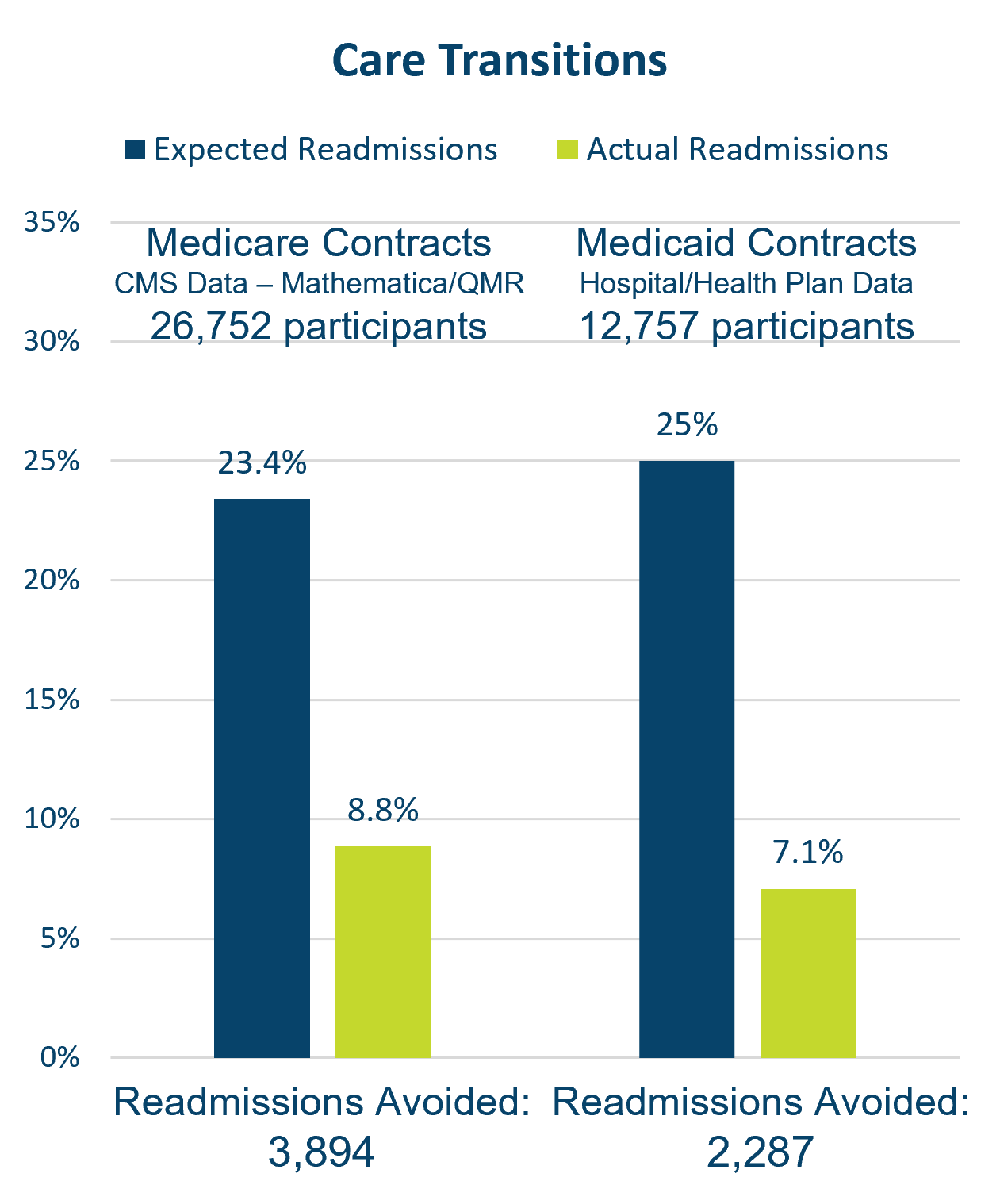
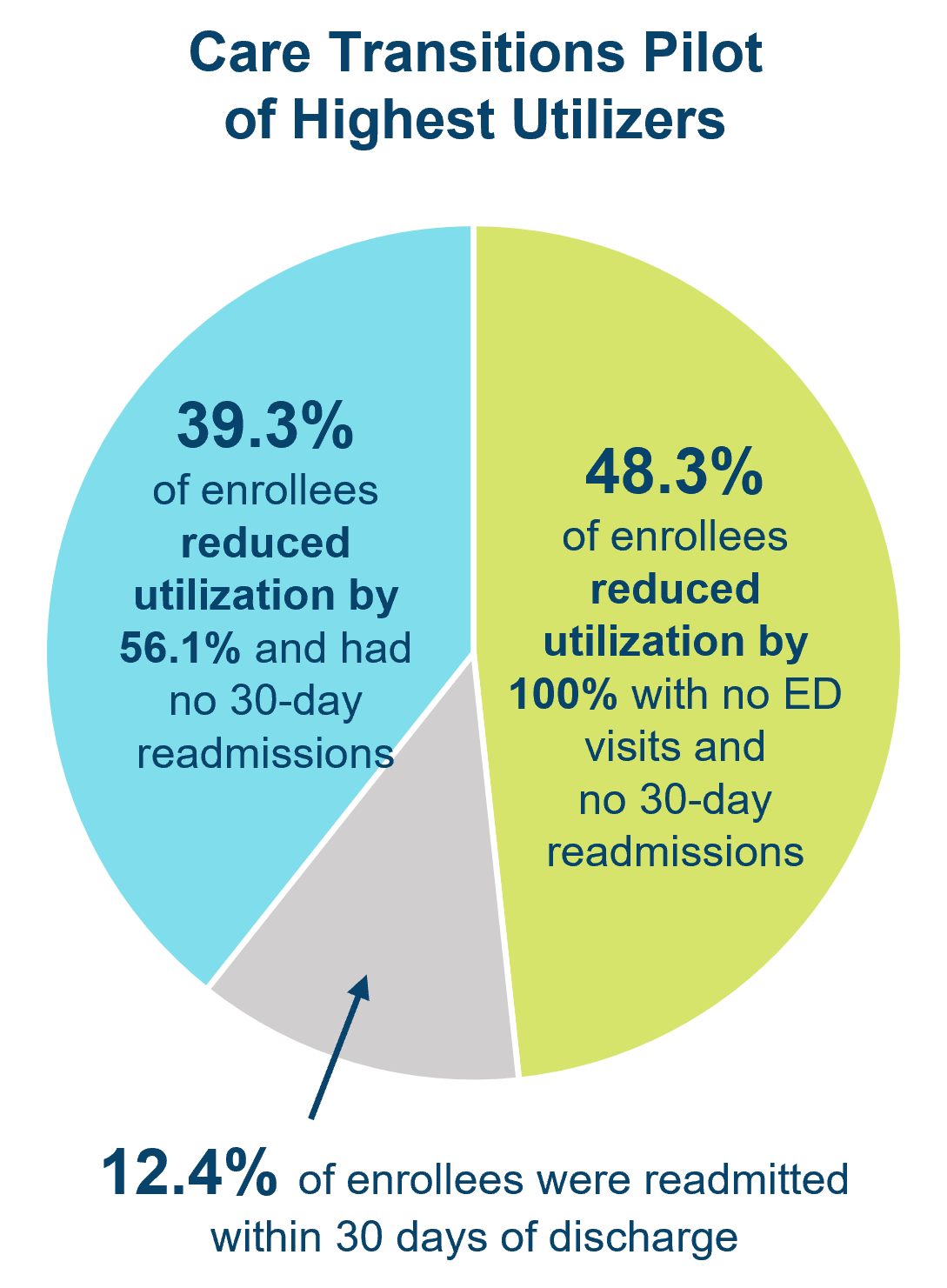
Our experienced staff has delivered care transitions since 2013 to over 45,000 Medicare and Medicaid patients, effectively reducing 30-day readmissions. Prior to the pandemic, we utilized the Care Transitions Intervention® model pioneered by Dr. Eric Coleman. We now follow the Transitional Care Support model, which can be customized to meet clients’ requirements with telephonic and telehealth options.
Services delivered in the home and community to address transportation issues, food insecurity, housing, and social isolation, as well as programs to manage chronic disease, prevent falls, and more, are proven supports that maximize independence and allow older adults to age in place.
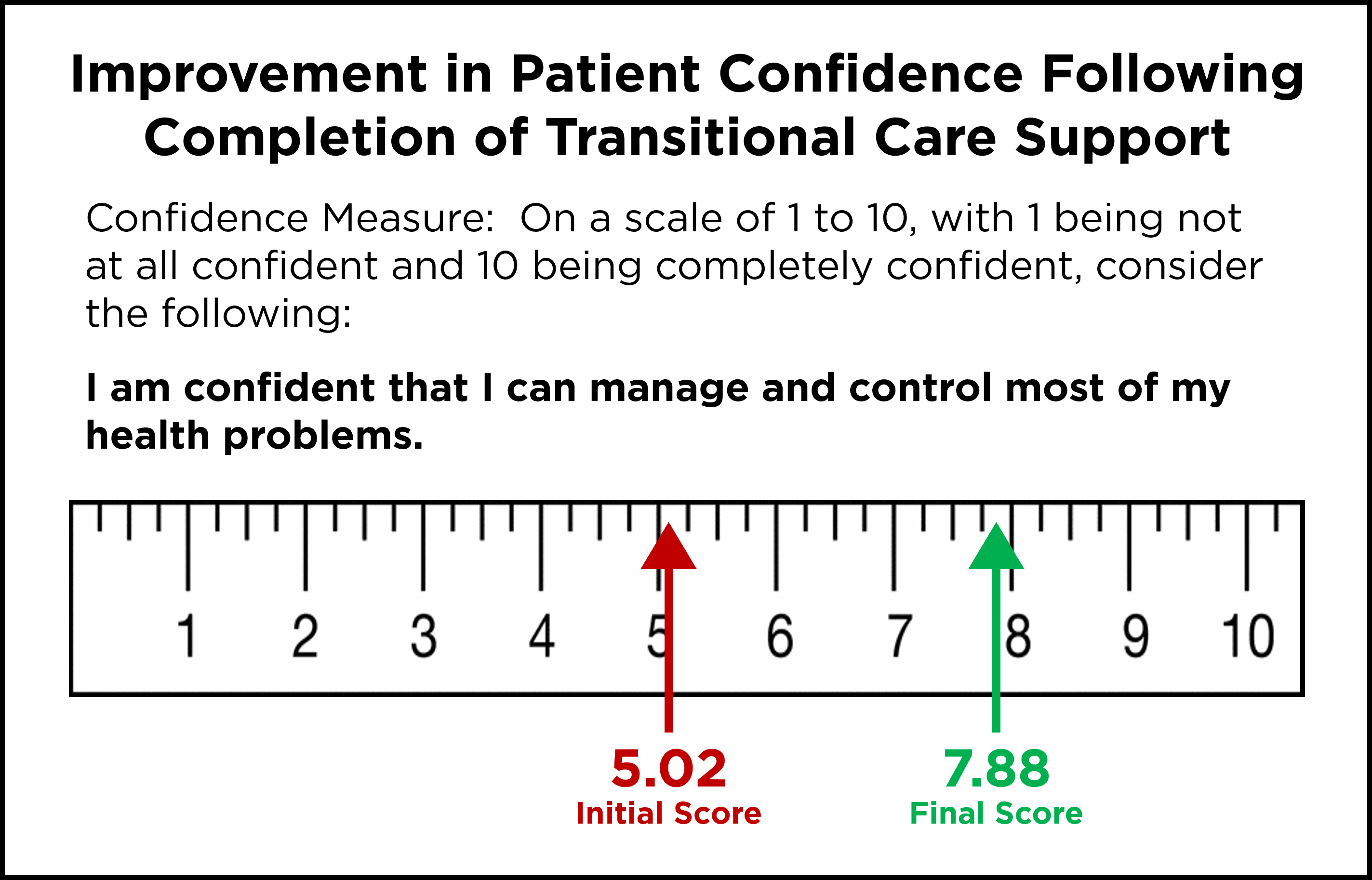
Transitional Care Support and Care Coordination empower patients, equipping them with the skills and insight needed to better manage their conditions. A survey of patients found that confidence in managing health problems, on a scale of 1 to 10, increased from 5.02 at the beginning of the intervention to 7.88 after completing the program.
VAAACares® Care Coordinators demonstrate consistent and successful member outreach and engagement completing MCO Member Health Screening (MMHS) assessments.

